When you’re experiencing health problems, the first step to getting the help you need is the right diagnosis. If you have a phobia, though, it’s highly likely that you’ll know which condition you have without needing to consult a medical professional. Nevertheless, if you’re seeking help for your condition, it can be helpful to have some form of diagnostic tool to turn to. Enter self-reporting for acrophobia.
Self-report instruments can help you to determine whether it’s likely that you have acrophobia. They can also enable you to understand how severely this phobia impacts your life. This information can be invaluable in ensuring that any treatment plans are suitable for your needs. However, there are some limitations to self-reporting that you’ll also need to take into account. In this article, we’ll explain more about how these tools work and outline their pros and cons.
What is self-reporting?
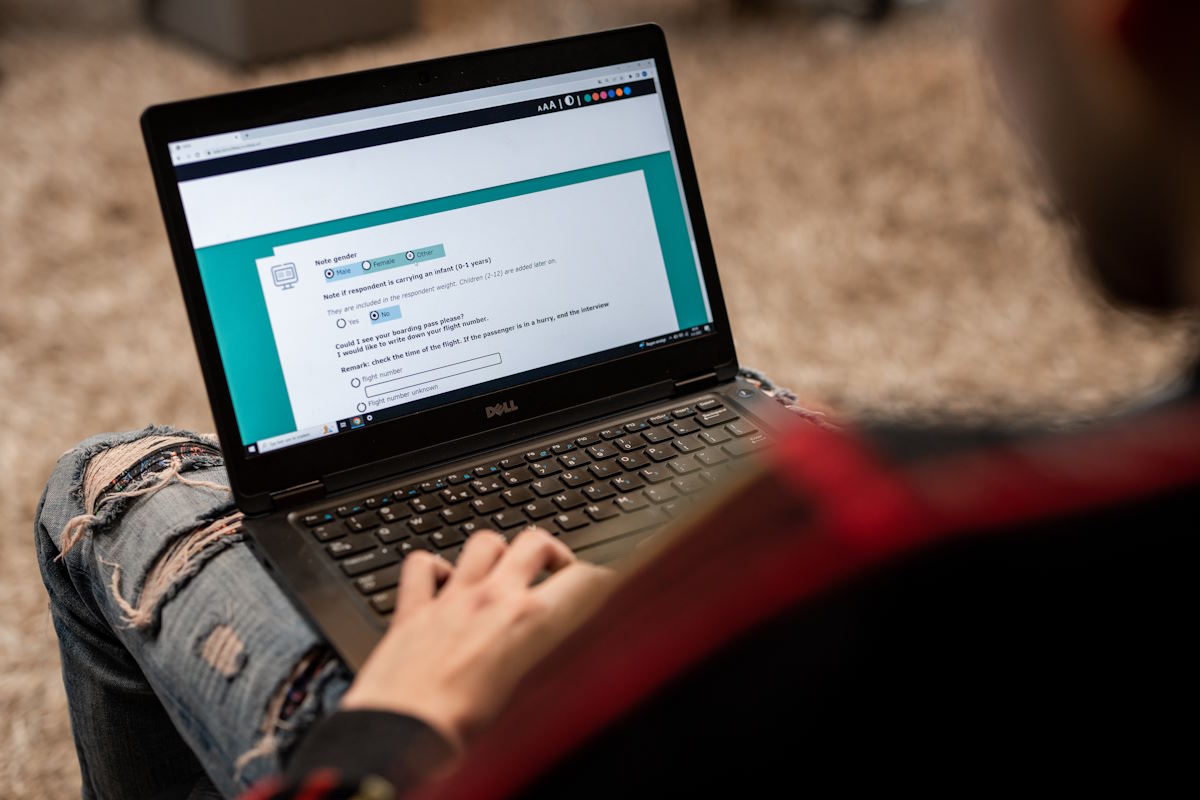
Self-reporting is a common method used as part of the process of diagnosing a range of mental health conditions. Most commonly, it involves the patient completing a questionnaire. A typical self-reporting questionnaire may consist of asking a patient how often they have experienced certain symptoms over a period of time—for example, the past week, two weeks or month.
Patients complete self-report questionnaires on their own, without the presence or input of a professional. They are designed to be easy and quick to fill out, with both paper and online versions available. This makes it possible for a patient to be assessed without needing to attend a hospital or doctor’s office. Additionally, because they provide patients with a numerical score, it’s possible to use self-report questionnaires to track progress over time.
Self-reporting for acrophobia

Acrophobia is the medical term for a phobia of heights. It is one of the most common phobias, and it can develop at any age. As it relates to a certain situation or activity, it is classed as a specific or simple phobia. This contrasts with complex phobias, which revolve around more deeply-rooted fears or anxieties.
Because acrophobia is a specific phobia, self-report questionnaires are suitable as a diagnostic tool. That’s because, according to a paper from Lancet Psychiatry, “specific phobias can be diagnosed with only a few questions”. This contrasts with more complex mental health conditions which may require medical observation.
It’s important, however, to understand both the benefits and the drawbacks of self-reporting. Below, we’ll discuss the pros and cons.
The positives
We’ve already discussed one of the key pros of using self-reporting for acrophobia: ease-of-use. All the patient needs to do is complete a short questionnaire, a process that takes mere minutes and requires no expert knowledge. This can happen on-site or remotely, allowing the patient to save on travel costs.
As mentioned above, it is possible to get an accurate diagnosis for a specific phobia, including a fear of heights, using a self-report questionnaire. It is therefore a more time and cost-effective method than requiring a patient to come into a doctor’s office.
Additionally, self-reporting offers medical professionals the chance to learn about how their patient reacts in certain situations without having to recreate them. For example, they can ask the patient to rate their fear when standing on a balcony without needing to see them do so. This has the benefit of reducing distress on the part of the patient, allowing for a more ethical approach to diagnosis.
The negatives
While self-reporting has numerous pros, it’s important to be aware of its potential downsides, too. The first of these is that, to be accurate, patients need to be honest. One factor making this difficult is social desirability bias. This is where respondents give answers that they deem to be ‘acceptable’ rather than telling the truth. A paper published in Addictive Behaviours notes that “social desirability response bias may lead to inaccurate self-reports”. Similarly, patients may feel too embarrassed to admit the extent of their phobia.
A variety of other considerations can affect the way that patients answer self-report questionnaires. First, there’s the questions themselves, which may—individually, or taken as a whole—impact upon the way a patient responds. Then, there’s the way individual brains work: some people are more naturally inclined to give ‘extreme’ or ‘moderate’ answers when using numerical scales, or be more likely to respond affirmatively or negatively to simple yes/no questions. Even a patient’s mood can affect their responses, with those feeling bad on the day they take the questionnaire being more likely to choose negative options.
Questionnaires used to diagnose acrophobia
If you’re interested in learning which tools are used to diagnose acrophobia, you’ll be pleased to learn that there are several questionnaires available. Below, we’ll provide quick overviews of a few of these measures.
Acrophobia Questionnaire (AQ)
One of the oldest available self-report measures used to diagnose a phobia of heights is the Acrophobia Questionnaire. Created by David C. Cohen in 1977, it actually consists of two subscales: AQ-Anxiety and AQ-Avoidance.
In the AQ-Anxiety subscale, the participant is presented with a list of 20 “situations involving height”. Examples range from “standing on a chair to get something off a shelf” to “riding a Ferris wheel”. They must then score each situation from zero to six, where zero indicates a situation where they feel “not at all anxious” and six indicates feeling “extremely anxious”. Total scores range from 0 to 120.
The AQ-Avoidance subscale reuses the same list of 20 situations. Here, however, the participant must state whether they would not avoid each situation, try to avoid it, or would not do it under any circumstances. These three answers correspond respectively to a score of 0, 1 and 2. Total scores range from 0 to 40.
Heights Interpretation Questionnaire (HIQ)
Published in 2011, the Heights Interpretation Questionnaire was created by Shari A. Steinman and Bethany A. Teachman of the University of Virginia. Those completing this questionnaire have to read about two height-related scenarios and imagine themselves experiencing them.
The first scenario relates to climbing a ladder leaning against a two-storey house. Meanwhile, the second asks the patient to envisage themselves on a balcony on the fifteenth floor of a building.
In each case, the patient is asked to rate the likelihood of certain things happening from 1 (not likely) to 5 (very likely). Examples include “You will fall”, “You will panic and lose control” and “You will faint”. Crucially, these ratings need to take into account the mindset the patient would have in that situation, rather than at the time of taking the survey.

Visual Height Intolerance Severity Scale (vHISS)
One of the newer measures used to diagnose this phobia is the Visual Height Intolerance Severity Scale, or vHISS. This questionnaire was first proposed by researchers Doreen Huppert, Eva Grill and Thomas Brandt of Ludwig-Maximilians-University in 2017.
vHISS focuses on both acrophobia and the related phenomenon of visual height intolerance (vHI). A 2013 study by the same researchers estimated that the latter condition, which “occurs when a visual stimulus causes apprehension of losing control of balance and falling from some height”, affects around one third of the population.
This questionnaire is a bit more complex than those listed above. It begins with a screening question, asking if the patient has ever experienced vHI. If they have not, they do not need to answer any further questions. If they have, they then answer six questions relating to the impact that vHI has had upon their life, its severity, and the length of time the symptoms have lasted. After these six questions, the patient is presented with two lists. The first is a range of physical symptoms, while the second is a set of scenarios which may trigger one’s vHI.
Two final questions are used specifically as part of the diagnosis of acrophobia: one relating to “fear when exposed to heights” and another about whether the patient avoids exposure to heights. If they answer both of these questions with a “yes”, and experience trembling, palpitations, inner agitation, sweating/moist hands and two other physical symptoms, then they can be diagnosed with acrophobia.
Next steps

Taking a self-report questionnaire to diagnose your acrophobia can be just the beginning of your journey. Once you know that you have a phobia of heights, the power is in your hands to do something about it.
If you’re ready to overcome acrophobia, then Climb Above Fear can help. When you book our course, you’ll be able to work with a therapist to learn more about the causes of your phobia, as well as to work to change the way you think about heights for good. To get started, contact Climb Above Fear today.



